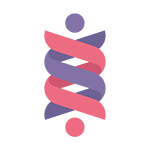
Sleep Statistics
The Centers for Disease Control and Prevention (CDC) in the United States has declared insufficient sleep a “public health problem.”
Did you know?
• 1 in 3 Americans Don’t Sleep Enough
According to the CDC, more than a third of American adults are not getting enough sleep on a regular basis.
• 1 in 4 Americans Develop Insomnia Each Year
According to the National Institute of Health, studies across the globe show anywhere from 10% to 30% of the population struggles with insomnia, defined as the consistent difficulty falling asleep and the inability to return to sleep after going to bed.
• Our Sleep is Getting Worse
According to recent evidence, the proportion of people getting less than the recommended hours of sleep is rising and is associated with lifestyle factors related to a modern 24/7 society, such as psychosocial stress, unbalanced diet, lack of physical activity and excessive electronic media use, among others.
• High Schoolers Get Too Little Sleep
According to the National Sleep Foundation, more than 87 percent of high school students in the United States get far less than the recommended hours of sleep, and the amount of sleep they get is decreasing, posing a serious threat to their health and academic success.
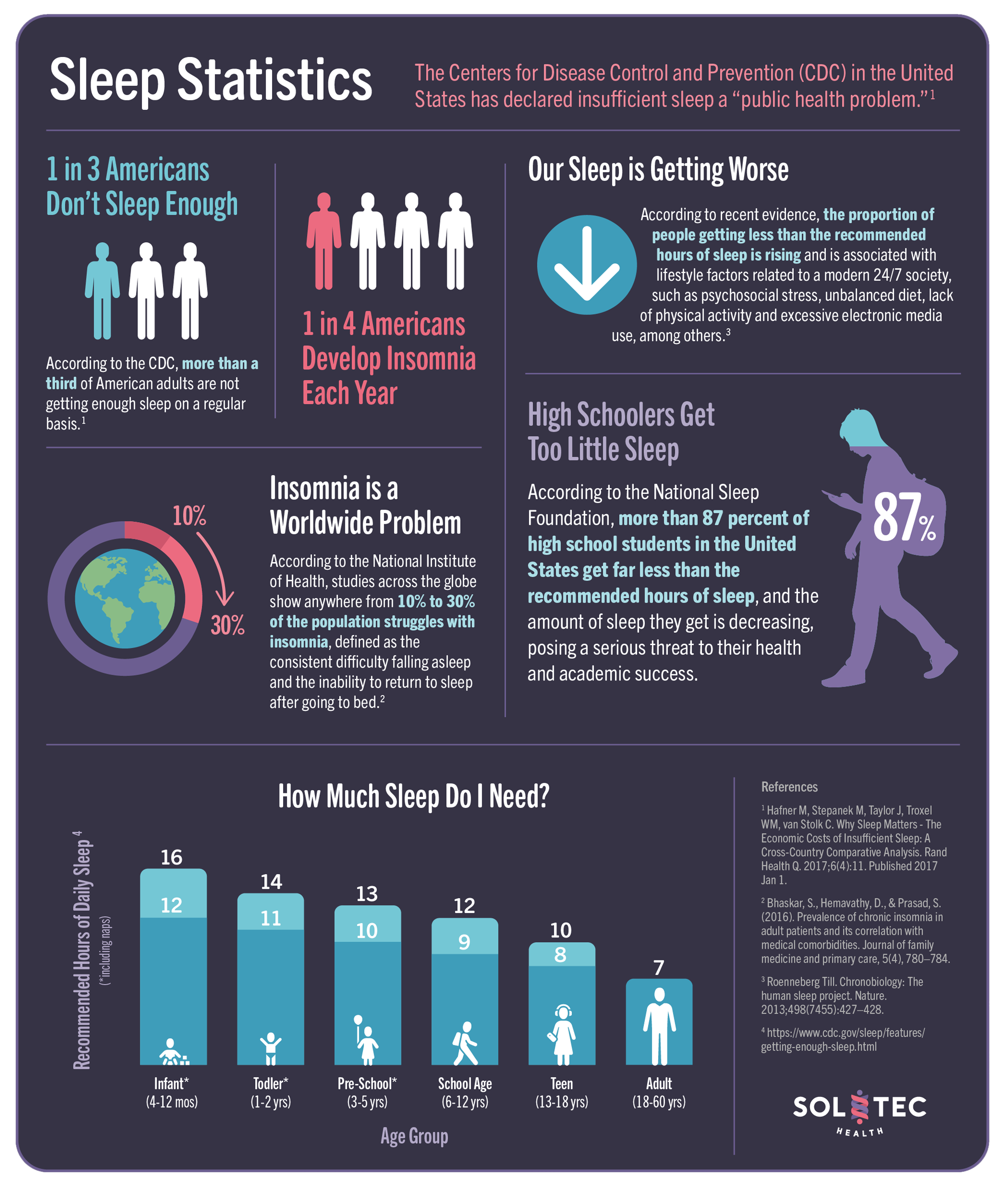
Health Impacts of Insufficient Sleep
Less Sleep Linked with 7 Out Of 15 Leading Causes of Death
Insufficient sleep duration has been linked with seven of the fifteen leading causes of death in the United States, including cardiovascular disease, malignant neoplasm, cerebrovascular disease, accidents, diabetes, septicemia and hypertension.
Less Than 6 Hours Of Sleep Increases Mortality Risk by 13%
An individual that sleeps on average less than six hours per night has a 13 per cent higher mortality risk than an individual sleeping between seven and nine hours, which is considered as the healthy amount of sleep.
Economic Costs of Insufficient Sleep
Less Sleep = Missed Work
A person sleeping six to seven hours loses on average about 3.7 working days more per year.
Absenteeism Is Expensive
On an annual basis, the U.S. loses an equivalent of about 1.23 million working days due to insufficient sleep. This corresponds to about 9.9 million working hours.
High Economic Toll
The costs of insufficient sleep in 2020 for the U.S. range from $299 billion to $433 billion.

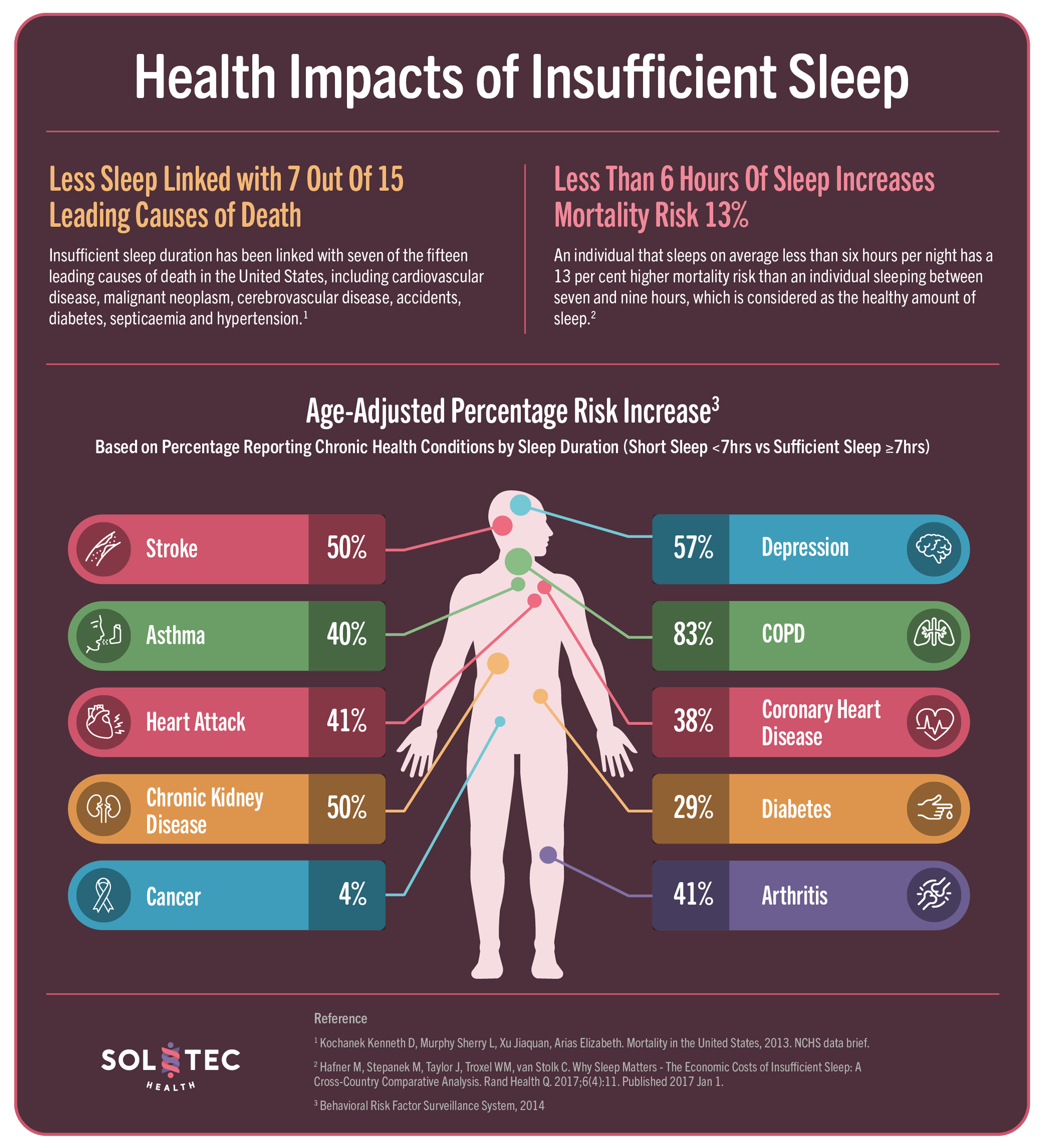
Gender and Aging
• Older Men Experience Less Slow Wave Sleep
Men over the age of 70 demonstrated a highly significant 50% reduction in slow wave sleep (SWS), relative to men under the age of 55, together with a concomitant increase in lighter NREM stages 1 and 2. In contrast, women showed no such significant decline in slow wave sleep or increase in lighter NREM sleep time relative to their younger gender group.
• Aging Affects How Soundly We Sleep
Advancing into the fifth decade of older age and beyond are a collection of well-characterized changes in sleep architecture: longer time taken to fall asleep, shorter overall sleep duration, more awakenings, arousals, or transitions to lighter sleep stages, reduced amount of slow wave sleep (SWS), increased time spent awake throughout the night.
• Men and Women Report Different Sleep Issues
According to the National Sleep Foundation (NSF) inaugural Sleep Health Index, women are more likely to report insomnia symptoms; men are more likely to say they snore, supporting previous data that have shown women are more commonly diagnosed with insomnia and men with sleep apnea.
• Menopause Affects Sleep
A growing body of evidence indicates that the development of sleep disorders following menopause contributes to accelerated cognitive decline and dementia in older women.
Daytime Activities Effect on Sleep
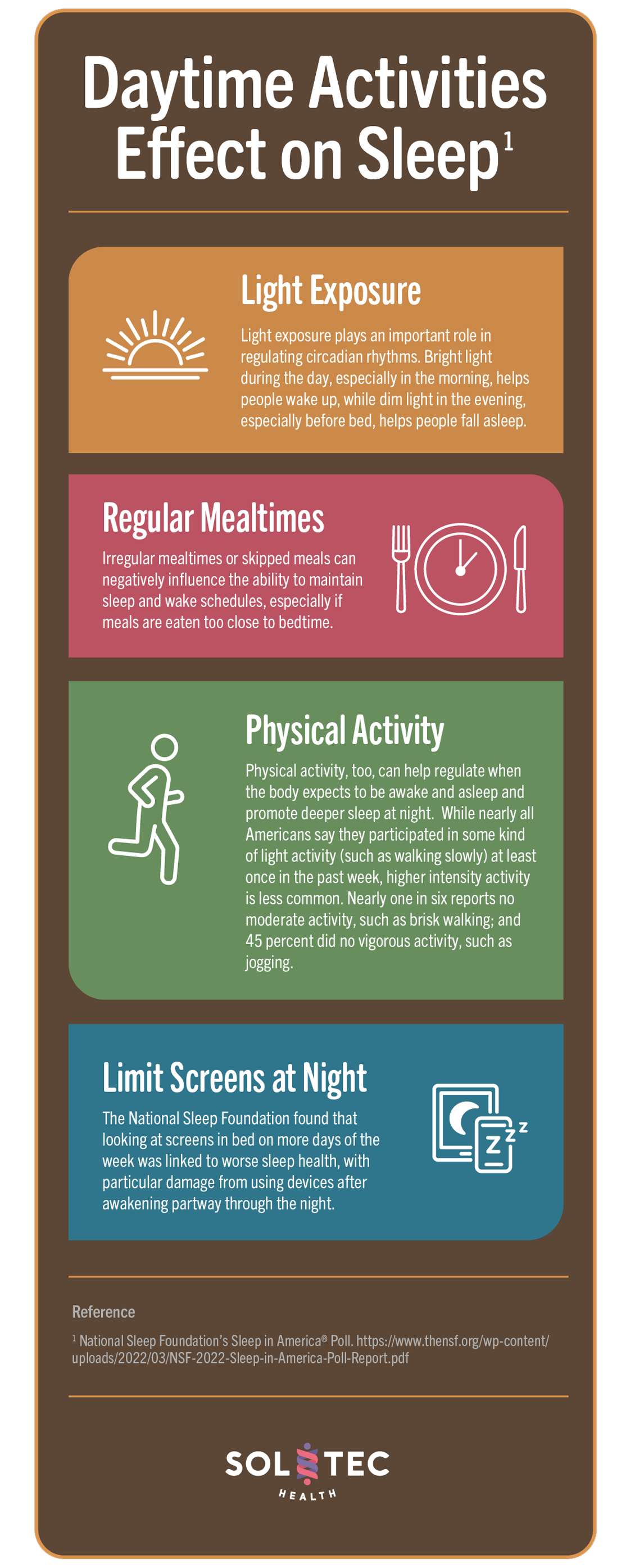
Light Exposure
Light exposure plays an important role in regulating circadian rhythms. Bright light during the day, especially in the morning, helps people wake up, while dim light in the evening, especially before bed, helps people fall asleep.
Regular Mealtimes
Irregular mealtimes or skipped meals can negatively influence the ability to maintain sleep and wake schedules, especially if meals are eaten too close to bedtime.
Physical Activity
Physical activity, too, can help regulate when the body expects to be awake and asleep and promote deeper sleep at night. While nearly all Americans say they participated in some kind of light activity (such as walking slowly) at least once in the past week, higher intensity activity is less common. Nearly one in six reports no moderate activity, such as brisk walking; and 45 percent did no vigorous activity, such as jogging.
Limit Screens at Night
The National Sleep Foundation found that looking at screens in bed on more days of the week was linked to worse sleep health, with particular damage from using devices after awakening partway through the night.
Time for a Nap?
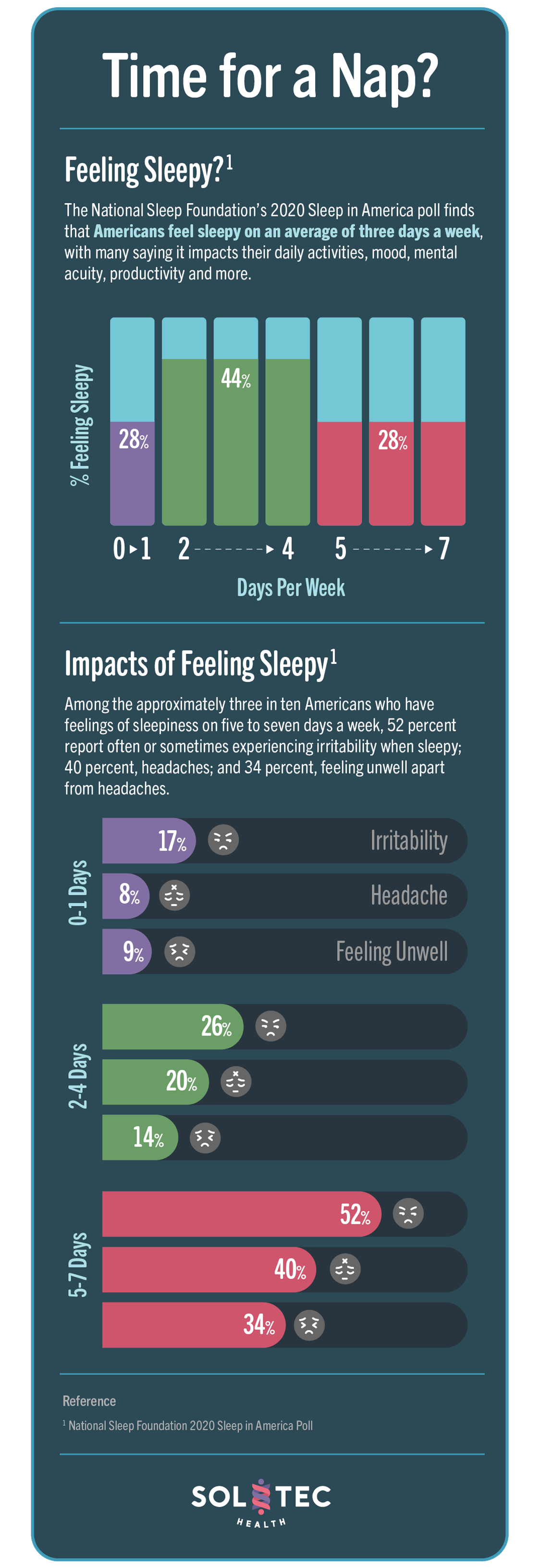
Feeling Sleepy?
The National Sleep Foundation’s 2020 Sleep in America poll finds that Americans feel sleepy on an average of three days a week, with many saying it impacts their daily activities, mood, mental acuity, productivity and more.
Impacts of Feeling Sleepy
Among the approximately three in ten Americans who have feelings of sleepiness on five to seven days a week, 52 percent report often or sometimes experiencing irritability when sleepy; 40 percent, headaches; and 34 percent, feeling unwell apart from headaches.
Sleep and the Pandemic

As the pandemic has unfolded, researchers have demonstrated that COVID-19 has had serious effects on sleep.
Trouble Sleeping
Around 40% of people have experienced sleeping problems, and studies have detected notable increases in insomnia symptoms in adults1 and children and adolescents.
More Anxiety
The pandemic has been found to increase the prevalence of anxiety disorders. Long before the pandemic, it was well-established that anxiety can disrupt sleep as a racing mind keeps the body tossing and turning.
Increased Insomnia
In a study conducted in China, the data suggested a 37% increase in the rates of clinical insomnia (from 14.6% to 20%) from before to peak of COVID pandemic.
The SOLTEC•HEALTH System is not intended to diagnose, treat, cure or prevent disease and should not be used as a substitute for professional medical advice, diagnosis or treatment. All content available through the products and services of SOLTEC•HEALTH is for general informational purposes only. This product and system protected by one or more of the following patents: U.S. Pat. Nos. 9,949,004; 11,478,604; and other U.S. and foreign patents pending and issued.